Key Takeaways
-
Fat transfer is a fascinating, artistic, and innovative surgical procedure that utilizes your very own fat. Not only does it restore volume and improve contours, it is solving cosmetic and medical concerns—including lymphedema. Natural & regenerative In recent years, fat grafting has been increasing in popularity for its natural, regenerative qualities.
-
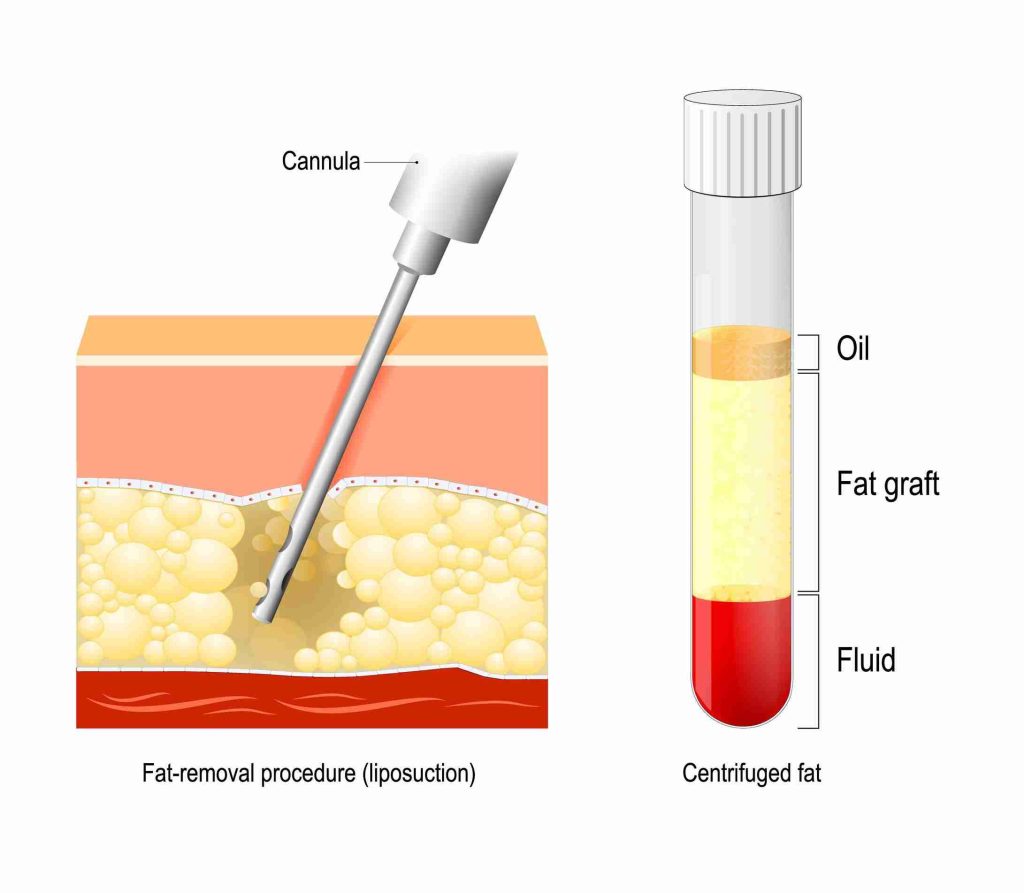
The technique consists of harvesting fat via liposuction, purifying it, and reinjecting it into areas of need. As with any graft or flap, adequate vascularization and lymphatic support are key to long-term success.
-
Fat transfer has many advantages, including natural looking results, very little downtime, and longer-lasting improvements than synthetic options. Its use is in harmony with the principles of regenerative medicine.
-
Fat transfer, too, offers a radical reduction in swelling for lymphedema patients. It stimulates lymphatic flow and improves the aesthetic/functional appearance of affected limbs, thereby making it integral to a multi-faceted and comprehensive treatment regimen.
-
Fat transfer is truly miraculous in reconstructive applications. It re-establishes volume and improves aesthetics for breast reconstruction, scar revision, and restoration of facial contour while accelerating the healing process.
-
To ensure the best outcomes, patients should choose an experienced surgeon, follow pre- and post-operative guidelines, and maintain realistic expectations about the procedure’s results and limitations.
Fat transfer is an artistic, innovative tool in the management of lymphedema in addition to the support of numerous other reconstructive applications. This strategy reuses a patient’s own fat to address both functional and cosmetic issues. It improves the cosmetic appearance of the affected area.
In the case of lymphedema, fat transfer reduces swelling and improves mobility, providing an overall better quality of life for patients who are looking for a long-term solution. In reconstructive applications, it’s mostly employed to restore volume and symmetry, often after surgeries such as mastectomy or trauma.
The operation begins with liposuction from areas such as the abdomen or thighs. Then, experienced specialists artfully inject that fat to enhance the desired areas. Its limited invasiveness and versatility further add to its appeal, cementing fat transfer as an indispensable resource in contemporary medicine.
What Is Fat Transfer
Fat transfer, or fat grafting, is a complex and still-developing surgical specialty that has gained prominence in recent years. Surgeons are expertly able to remove adipose fat, commonly referred to as fat, from a specific area of the body and deposit it into another. This powerful technique can be used for a wide range of cosmetic and reconstructive needs, including fat transfer surgeries for lymphedema treatment.
Then, in 1893, German plastic surgeon Gustav Neuber took a radical step. He was the first to use fat transfer to repair scars around the eye from an infection. This marked a significant milestone in the evolution of fat transfer techniques, paving the way for modern applications such as vascularized lymph node transfer.
In the field of reconstructive surgery, fat transfer is essential to the advancement of facial rejuvenation and treatment of lymphedema. Fat grafting helps restore lost volume and improves the look of chronic wounds or scarred areas. It offers patients a natural-looking enhancement and helps promote the health of the tissue underneath.
For lymphedema patients, it helps to restore their lymphatic systems and provides both functional and aesthetic benefits. This dual advantage makes fat transfer a valuable option in reconstructive procedures, especially when combined with techniques like lymphaticovenular anastomosis.
Regenerative medicine has started to embrace fat transfer techniques with open arms. That’s because fat is full of mesenchymal stem cells (MSCs) that are 300-500 times more plentiful than in bone marrow. MSCs have inherent immunomodulatory properties that actively promote tissue repair and healing, making fat graft survival highly effective.
This is why fat grafting is currently a highly effective treatment for breast cancer-related lymphedema, among other medical conditions. The integration of fat transfer into regenerative medicine highlights its potential for broader applications, including cosmetic surgery and lymphedema surgery.
Fat transfer has become increasingly common in cosmetic procedures such as breast and facial augmentation in recent years. With its biocompatibility and long-lasting results, it shows its trustworthiness. Additionally, it has low complication rates, with a 27.8% complication rate in breast related procedures illustrating its efficiency.
This growing popularity underscores the effectiveness and safety of fat transfer in both cosmetic and reconstructive surgery, making it a preferred option for many patients seeking aesthetic enhancement or surgical treatment for lymphedema.
Fat Transfer for Lymphedema
1. How It Treats Lymphedema
Fat transfer alleviates swelling, improves lymphatic flow, and provides tissue restoration in lymphedematous limbs to give the appearance of a healthy limb. The transplanted fat is infused with hyaluronic acid (HA) and stem cells. This powerful blend works in conjunction with the body’s natural lymphatic repair and has the ability to stimulate new lymphatic vessel growth.
These adaptations greatly increase lymphatic propulsion. In addition, they mitigate fluid accumulation, with histological analysis showing a marked increase in the lymphatic transport index, achieving 12.8 in the long run. Patients immediately experience aesthetic benefits with improved contouring, smoother skin, and an overall enhanced appearance of the limb.
Specifically, at 6 months after the procedure, general appearance scores were an average of 7.2, indicating marked cosmetic improvements. Impressive and lasting results long-term follow-ups show one case achieved a spectacular reduction of 358 mL, or 10%, in arm volume at 64 months of follow-up, and reported a reduced requirement for compression garments.
These outcomes combined lead to a greatly improved quality of life for people living with lymphedema.
2. Techniques Used for Lymphedema
Advanced harvesting techniques with the liposuction devices are necessary to harvest fat from lymphedema patients due to their large fat stores and adipogenic potential. They harvest your fat that is rich in anti-aging molecules. Then, they re-inject it using techniques such as fanning or cross-hatching to ensure uniform dispersion.
Increased accuracy through the use of pre-marking injection sites and improvements in surgical tools create a safer, more efficient process. These approaches aim to optimize graft retention, even at the 20%–50% resorption rate seen with the best methods.
3. Recovery Process for Patients
After recovery from fat transfer varies but usually takes a few weeks. Educating patients on the importance of post-operative care, such as wearing compression garments and managing swelling are key components. Physical therapy, including exercises and lymphatic drainage, might be advised to promote mobility and stimulate lymphatic system repair.
Consistent follow-ups help to keep progress on track, as well as any worries you may have to keep them in check. Patients usually enjoy lifelong benefits, swelling is reduced and functioning of the limb is improved.
4. Expected Outcomes and Results
Patients can look forward to significant changes to their limb’s volume and normal skin appearance. For example, one patient had almost complete breast symmetry and very little swelling 64 months after the procedure. Satisfaction studies emphasize those down-to-earth results, with at times multiple procedures required for best effects.
We find not only that the overall quality of life increases, but that it is accompanied by decreased compression garment dependence and improved limb function.
Reconstructive Applications of Fat Transfer
Enhancing Breast Reconstruction
Fat transfer is increasingly recognized as a key adjunct in improving the outcomes of breast reconstruction following mastectomy. Surgeons use autologous fat grafting to help the breast regain its natural contour and volume. This technique not only restores symmetry, but architectural form and beauty as well.
This technique beautifully complements the results of implant-based reconstruction. By using fat, it smooths jagged edges, providing a gentler, more organic contour. Fat grafting has many beneficial effects, including rejuvenating skin quality, improving scarring, and helping tissues that have been damaged by radiation therapy.
A patient with previous mastectomy and radiation therapy obtained excellent symmetry and profile improvements. These benefits were still observed at a 64-month follow-up. The approach of micropurifying fat droplets before injecting them in multiple micro-layers guarantees higher graft survival and no complications such as necrosis.
Improving Facial Contour Restoration
Facial rejuvenation and restoration of facial contour loss due to volume depletion are some of the most frequent reconstructive applications of fat transfer. This artistry technique of strategic placement works to replace lost volume and bring back the youthful fullness to cheeks, temples, and other hollowed areas.
Autologous fat is biocompatible and provides results that are long-lasting. It shouldn’t be surprising that it improves skin quality due to the large number of mesenchymal stem cells it contains. Fat grafting can correct even the most severe facial deformities.
It provides a very natural and balanced appearance by restoring symmetry due to trauma or congenital conditions.
Correcting Scars and Deformities
Fat transfer is essential in softening all scars and correcting scars and deformities. Its regenerative properties enhance tissue integration and healing. This renders it the ideal modality for restoring the texture and contour to scarred regions.
Congenital deformities and trauma-related injuries are both areas where fat grafting can make a huge difference. This technique achieves a dual goal of restoring volume while stimulating local tissue repair. These studies demonstrated promising outcomes with patients claiming improved function and aesthetics in previously scarred areas.
The ability to deliver these growth factors and other essential nutrients only serves to add to the benefits of fat transfer when it comes to reconstructive surgery.
Supporting Post-Trauma Recovery
Fat transfer is being acclaimed more and more as an important component of recovery from trauma. By restoring lost volume, it not only makes a patient look better, it helps promote greater functional rehabilitation of damaged tissues.
The high concentration of stem cells in adipose tissue speeds up healing processes, leading to a much better overall recovery. Multidisciplinary strategies often combine fat grafting with additional surgical procedures.
This approach maximizes what can be achieved and offers patients a more complete answer to the complex issues caused by trauma.
Benefits of Fat Transfer Procedures
Natural and Biocompatible Solution
Fat transfer is a natural and biocompatible tissue repair option, as it uses your own fat. Unlike synthetic fillers, which can carry a risk of rejection or allergic reactions, autologous fat is accepted naturally by the body. Doing so decreases the likelihood of complications and facilitates a more natural integration with nearby tissues.
This is largely because adipose tissue, or body fat, is abundant in stem cells, which are known for their regenerative properties. These cells can help to heal injured tissues, including long-standing wounds or tissue injured by radiation therapy. Fat grafting has been proven to help scars from osteomyelitis or radiation damage.
This is in harmony with regenerative medicine principles and provides a more holistic approach to patient care.
Long-Term Results and Durability
Fat grafting offers more permanent results than synthetic fillers. Clinical studies have reported retention rates of 47%–65% for breast fat transfer and 40% for facial grafting. We have patients who, several years out, are still thrilled, with little to no requirement for touch-ups.
Breast implant removal with fat replacement has pioneered astonishing long-term outcomes. Most patients are thrilled with these results without requiring additional appointments. With fat’s natural integration, volume and contour improvements are long-lasting, and maintenance is as easy as simple, non-invasive periodic touch-ups.
Minimal Risk of Rejection or Allergies
Since you’re using your own fat, the risks are reduced. When performed with proper technique, the procedure is safe, even in areas considered to be high-risk.
Fat grafting for postmastectomy lymphedema and chronic scars has been used safely and effectively, proving its reliability.
Potential Risks of Fat Transfer
Common Side Effects After Surgery
You may notice a few common side effects. These are all minor and temporary procedures, ranging from swelling, bruising, and tenderness at the donor and recipient sites. These symptoms are common, temporary, and normal signs of the body’s healing, typically resolving within a few weeks.
Most patients experience a dramatic resolution of swelling and bruising within two to three weeks. Some can develop moderate swelling that lasts for three or more months. Be diligent about following your post-operative care instructions.
Do not apply compression garments to the graft site for at least four weeks to limit adverse effects and improve your healing process. It’s important that patients know what normal recovery looks like, including what’s normal—a little discomfort.
They must be educated on how to identify abnormal symptoms like ongoing pain or redness, which may signal complications.
Rare Complications to Be Aware Of
Though uncommon, serious complications may develop including fat necrosis, infection, or contour irregularities. Based on the most recent literature, the combination of fat necrosis and asymmetry, including contour deformity, occurs in an estimated 14.4% of patients.
Infection occurs in only 1.8% of cases. These risks are reduced with the application of proper surgical techniques and careful patient selection. For instance, avoiding high negative pressure during liposuction allows for better preservation of the fat cells and less trauma, which in turn lowers complications.
Carefully coordinated, frequent follow-up visits are necessary to keep a close eye on recovery and catch complications, if any, early.
How to Minimize Risks Effectively
Minimizing risks begins with choosing a skilled surgeon who specializes in fat transfer procedures. Preoperative assessments help identify any risk factors, ensuring patient safety.
Overfilling by 20%, as recommended by experts, accounts for natural fat absorption and improves long-term results. Strictly following post-operative care guidelines, such as keeping the graft site free from pressure and adhering to activity restrictions, supports recovery.
Preparing for a Fat Transfer Procedure
Consultation with Medical Professionals
A thorough consultation with your physician will be your best starting point to prepare for a fat transfer procedure. This conversation should include a comprehensive review of your medical history and current health status. This allows them to pinpoint any possible risks and make sure you’ll be safe.
Clear, open communication is the key. If you share your expectations and desired outcomes, your doctor will be able to develop a customized treatment plan tailored specifically to you. If you are considering fat transfer for lymphedema, your provider will focus mostly on the areas most impacted.
This specialized, lymphatic-focused technique is designed to improve your lymphatic function. Consultations allow for the identification of any contraindications, such as underlying health issues or lack of available fat for harvesting. Taking care of these things ahead of time paves the way for a smoother process.
Preoperative Instructions to Follow
Patients should follow these essential steps before lymphedema surgery, including understanding the importance of fat transfer surgeries and the role of lymphatic vessels in recovery.
-
Do not take any blood-thinning medications such as aspirin, ibuprofen, or warfarin for a minimum of two weeks before your procedure.
-
Begin nutritional supplements such as HealFast and Juven as prescribed by your physician. These stimulate healing and provide faster recovery times.
-
Drink plenty of water and consume a healthy diet to nourish your body.
-
You will need help after surgery.
-
Follow fasting instructions carefully for optimal surgical safety.
Understanding the Procedure’s Limitations
Fat transfer does have its limitations. How much fat can I harvest depends on my body type. On top of that, graft survival rates vary widely from individual patients.
Age, health, and lifestyle all play a role in the outcome as well. While swelling is normal, it is not permanent and there are some distinct limitations, e.g. No pressure to grafted areas, that lead to optimal outcomes.
Realistic expectations are the key to being happy with any type of procedure.
Who Can Benefit from Fat Transfer
Fat transfer provides an incredibly versatile solution for almost anyone. Patients who develop lymphedema symptoms generally experience damage or obstructions to their lymphatic system. Fortunately, fat grafting can offer relief by restoring elasticity back into the tissues and eliminating pain and irritation associated with lymphedema fat.
For individuals reclaiming their bodies after trauma or those who have grown up with congenital deformities, fat transfer is an astounding functional and aesthetic option. For example, this technique is quite successful in repairing scarring from osteomyelitis or radiation damage. Damaged tissue can flourish due to the regenerative properties of the fat stem cells contained in fat grafts.
Outside of the medical arena, fat transfer has become increasingly popular among patients looking for natural-looking cosmetic improvements. Unlike many synthetic fillers, fat grafting utilizes the patient’s own tissue, providing a safer and more sustainable option for those seeking plastic surgery.
This is particularly sought after by people in the Chicago area correcting facial volume loss or breast asymmetry. Research found that fat transfer can increase an average of about 140.6 grams per breast, allowing patients to obtain a more symmetrical look. Of course, its uses have outgrown these initial applications and it has been utilized to rectify post-mastectomy complications, including asymmetry or scarring.
Fat transfer is inclusive across various demographics, as it can cater to young adults dealing with trauma scars, middle-aged individuals seeking natural rejuvenation, or older patients requiring reconstructive care. Its flexibility makes it easier to implement and therefore more enticing to a range of actors.
Ideal Candidates for the Procedure
Ideal candidates for fat transfer are usually people who are in good overall health with realistic expectations. They should have localized fat deposits amenable to harvest and areas in need of volume restoration.
Additionally, patients with post-mastectomy lymphedema could be helped by innovative flap reconstruction and fat transfer combination procedures. Psychological readiness is just as important, with knowing and being able to accept the commitment to healing and realistic outcomes being pivotal to success.
Comprehensive pre-procedure evaluations, such as a review of a patient’s medical history and advanced imaging, allow qualified practitioners to determine ideal candidates and achieve optimal outcomes.
Conditions That Can Be Treated
Fat transfer surgeries effectively address a variety of conditions, including lymphedema fat issues.
-
Lymphedema and related tissue damage.
-
Breast reconstruction post-mastectomy, especially with LD flap techniques.
-
Facial volume loss from aging, trauma, or surgery.
-
Scars and deformities caused by accidents or previous operations.
Factors Affecting Treatment Success
Just a few of the factors that can determine the success of fat transfer are. The surgeon’s skill and experience play a vital role in successful procedure, as accurate handling guarantees a higher graft survival.
Patient compliance with post-operative care, such as not applying pressure to treated areas and adhering to aftercare instructions, is crucial, too. Whether or not the graft integrates well depends on the individual biological response to the graft.
Elements such as blood supply and fat absorption are major players in this process. For instance, stem cells found in adipose tissue may improve healing in areas damaged by radiation, adding to the positive outcome.
Conclusion
Fat transfer provides a feasible solution for treating lymphedema and supporting reconstruction. The outpatient procedure utilizes your own fat to enhance mobility, alleviate pain and give your body a more organic shape. It combines medical advantages with aesthetic enhancements, making it a versatile and appealing option for many.
The specific results achieved will vary based on each person’s needs and goals, with careful planning and attention, it can produce beautiful, natural-looking results. Consulting with an experienced, board-certified provider will help you determine if the process is right for you and make you feel confident about your decision.
If you’re planning to use fat transfer for lymphedema or other reconstructive applications, reach out and talk to an expert today to get started. Solid guidance and personalized, professional counsel ensure you’ll make the right choice for your health and well-being.
Frequently Asked Questions
What is fat transfer?
Fat transfer surgery is a cosmetic and increasingly common reconstructive procedure that utilizes your body’s own fat to restore volume and shape to targeted areas. This process involves harvesting fat from one site through liposuction techniques and transferring it to another site, highlighting the importance of fat graft survival for optimal results.
How can fat transfer help with lymphedema?
The procedure seems to enhance unhealthy tissue, reduce swelling severity in lymphedema patients, and improve lymphatic drainage, providing relief by repairing affected sites through innovative surgical interventions.
What are the reconstructive uses of fat transfer?
In addition to mastectomy patients, fat transfer surgeries are gaining ground as a form of breast reconstruction, facial rejuvenation, and scar treatment. This technique is perfect for volume restoration, symmetry improvement, and contour enhancement after trauma or surgery.
Who is a good candidate for fat transfer?
The best candidates for fat transfer surgeries are healthy individuals with sufficient lymphedema fat available and reasonable expectations. Consult a highly experienced specialist to ensure you are an appropriate candidate.
What are the benefits of fat transfer procedures?
Fat transfer surgeries provide natural results and minimal scarring, effectively addressing cosmetic and reconstructive needs while utilizing lymphedema fat for volume restoration and fat removal benefits.
Are there risks associated with fat transfer?
Of course, there are always risks such as infection, fat absorption, or lumpy results associated with fat transfer surgeries. Selecting a highly qualified plastic surgeon reduces these risks and makes the procedure a safe one.
How should I prepare for a fat transfer procedure?
Follow your surgeon’s instructions, such as staying off certain medications, stopping smoking, and living a health-oriented life to enhance fat graft survival and ensure optimal recovery.





