Osteoma removal is a critical procedure for those diagnosed with this benign but often bothersome bone tumor. Typically emerging on the skull, osteomas can cause discomfort or lead to cosmetic concerns, prompting individuals to seek effective treatment options. This guide aims to demystify the process of osteoma removal, shedding light on what patients can expect before, during, and after surgery. By understanding the techniques used by healthcare professionals and the recovery journey ahead, individuals facing this condition can approach their treatment with confidence and clarity.
Understanding Forehead Osteoma
Benign Tumors
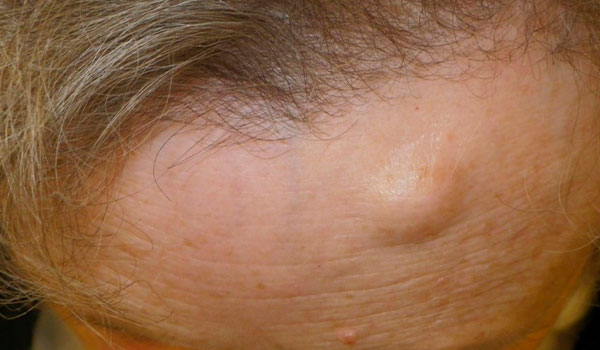
Osteomas are benign tumors. They grow on bones, often on the forehead or skull. These growths are not cancerous.
Mostly, adults find these lumps by their looks rather than pain. It’s rare for children to have them. The slow-growing nature of osteomas means they don’t cause immediate health issues.
Detection and Growth
People usually notice a small, hard lump on their forehead. This is how most osteomas are found. They grow slowly and don’t hurt.
Because they’re typically painless, many discover them accidentally. Perhaps when touching their forehead or looking in a mirror. Despite being harmless, some might wish to remove them for cosmetic reasons or discomfort caused by pressure on surrounding tissues.
Overview of Osteoma Treatment Options
Surgical Removal
Surgical removal stands as the most effective method for treating osteomas. This process involves a medical professional excising the tumor from the affected area. The goal is to eliminate all abnormal tissue while minimizing damage to surrounding healthy tissues.
The necessity for surgery largely depends on factors such as the osteoma’s size and its location on or within the body. For instance, an osteoma located on the forehead might require a different surgical approach compared to one situated deep within bone structures.
Minimally Invasive Options
Minimally invasive procedures offer an alternative with fewer risks and shorter recovery times. These methods include endoscopic surgery, where small incisions are made, and special instruments are used to remove the tumor.
This option is particularly appealing for patients seeking less visible scarring and those concerned about long recovery periods. It’s suitable for smaller tumors that are easily accessible.
Traditional Surgery
For larger or more complex osteomas, traditional surgery may be necessary. This approach provides surgeons with direct access to the tumor, allowing them to remove it completely.
Traditional surgery requires longer healing times and carries greater risk of complications compared to minimally invasive techniques. However, it remains a vital option when dealing with extensive tumors that cannot be addressed through other means.
Choosing between these treatment options involves considering several factors:
-
The osteoma’s size
-
Its location
-
The patient’s overall health
Doctors will recommend the best course of action based on these criteria, ensuring optimal outcomes while prioritizing patient safety.
Minimally-Invasive Surgery for Osteoma
Small Incisions
Minimally-invasive surgery involves small incisions. This means less tissue is disturbed during the procedure. Surgeons use specialized tools to remove osteomas through these openings.
The benefits are clear. Patients experience less pain and swelling post-operation. There’s also a reduced risk of infection due to smaller wounds.
Quick Recovery
One major advantage is the shorter recovery time. Traditional surgeries often require weeks or even months for full recovery. With minimally-invasive techniques, patients can return to their daily activities much sooner.
This method is especially beneficial for removing small osteomas that have minimal cosmetic impact on visible areas like the face or arms.
Ideal Candidates
Not everyone is a suitable candidate for this type of surgery. It’s best suited for individuals with smaller osteomas that do not affect deeper structures beneath the skin.
Patients seeking minimal cosmetic changes find this option appealing. The likelihood of noticeable scarring is significantly lower compared to traditional surgical methods.
Endoscopic Osteoma Removal Procedure
Visual Advantages
The endoscopic approach to osteoma removal significantly enhances the surgeon’s ability to see the affected area. This technique involves using an endoscope, a small, flexible tube with a light and camera at the end. It allows for detailed visualization of the osteoma and surrounding tissues.
Surgeons can navigate challenging areas with greater precision. This is particularly beneficial for osteomas near sensitive structures like the supraorbital nerve. The enhanced view helps in avoiding damage to these critical areas during surgery.
Minimal Scarring
One of the most notable benefits of this procedure is its ability to minimize scarring. Since it involves smaller incisions than traditional surgery, patients are left with less noticeable scars post-operation. This aspect makes it an attractive option for those concerned about cosmetic outcomes.
Furthermore, due to precise dissection and resection facilitated by better visualization, there’s reduced trauma to surrounding tissues. This not only contributes to minimal scarring but also promotes faster healing and recovery times.
Forehead Osteoma Excision Techniques
Technique Selection
Selecting the right technique for forehead osteoma removal is crucial. The choice depends on the osteoma’s size and depth. For small, superficial osteomas, less invasive methods might be preferred. These can lead to quicker recovery times.
Larger or deeper osteomas require more complex techniques. Surgeons often use detailed imaging studies to decide the best approach. This ensures a balance between complete removal and minimal scarring.
Cosmetic Consideration
Cosmetic outcomes are a significant concern in forehead osteoma excision. Some methods prioritize aesthetics more than others do. Techniques that involve smaller incisions tend to leave less noticeable scars.
Surgeons may choose endoscopic procedures for their cosmetic benefits, especially following up from an endoscopic osteoma removal procedure discussed earlier. This method minimizes visible scarring by using tiny cameras and instruments inserted through small cuts.
Surgeon Expertise
The surgeon’s expertise plays a pivotal role in technique selection.
-
Experienced surgeons can handle complex cases more effectively.
-
They tailor their approach based on individual patient needs and cosmetic concerns.
Choosing a surgeon with specific experience in forehead osteoma excision is essential for achieving optimal results. They evaluate each case carefully, considering both medical necessity and patient preferences regarding post-surgical appearance.
Anterior Hairline Incision Method
Cosmetic Discretion
The anterior hairline incision method involves making a cut along the hairline. This is done for cosmetic reasons. The aim is to hide the scar within the natural lines of the scalp. It’s a smart choice when discretion is key.
This technique minimizes visible scarring after recovery. Patients often prefer this method for its subtlety. The scar blends with the hairline, becoming almost invisible over time.
Extensive Access
For larger osteomas that need more extensive work, this method shines. It provides wide access to the affected area without significant visible scarring. Surgeons can reach deeper layers effectively through subgaleal and subcutaneous dissection.
The process involves careful separation of layers down to the frontalis muscle. This ensures thorough removal of the lesion while protecting vital structures like facial nerves.
Recovery and Outcomes
Post-surgery care focuses on minimizing scarring and ensuring a smooth recovery.
-
Follow-up appointments are crucial.
-
Sutures are typically removed within a week.
-
Applying recommended ointments helps in healing.
Patients report high satisfaction rates due to minimal scarring and effective osteoma removal using this method.
Candidate Evaluation for Removal
Medical Assessment
The first step in evaluating a patient for osteoma removal involves a comprehensive medical assessment. This includes reviewing the patient’s medical history, conducting a thorough physical examination, and utilizing imaging studies such as CT scans. These diagnostic tools are crucial in determining the size, location, and characteristics of the osteoma.
Doctors consider several factors during this phase. Not every osteoma poses a health risk or requires immediate removal. In some cases, monitoring the growth over time may be advisable.
Decision Factors
In deciding whether to proceed with osteoma removal, both symptoms and risks play significant roles. Symptoms that cause discomfort or interfere with daily activities can prompt consideration for surgery. However, if an osteoma is asymptomatic—meaning it doesn’t cause symptoms—it might not need intervention.
Another critical aspect of the decision-making process involves evaluating potential risks associated with surgery versus the benefits it may bring. Doctors also take into account patient-specific factors such as lifestyle needs and cosmetic concerns which could influence their recommendation.
-
Pros of removal include relief from symptoms and improved cosmetic appearance.
-
Cons might involve surgical risks like infection or injury to nearby structures.
Ultimately, consultation with a double board-certified specialist at an accredited institute ensures that patients receive personalized advice tailored to their unique situation.
Post-Operative Care for Osteoma Removal
Wound Care
After osteoma removal, proper wound care is crucial. This involves keeping the area clean and dry. Patients should gently clean the wound as advised by their doctor.
Avoid applying pressure or rubbing the area. This helps prevent irritation of the periosteum, a layer surrounding bones where osteomas form.
Pain Management
Pain management is another key aspect of post-operative care. Doctors usually prescribe medication to ease discomfort. It’s important to take these as directed.
Over-the-counter pain relievers may also be recommended. However, always consult your doctor before taking any new medication.
Activity Restrictions
Patients must follow specific activity restrictions after surgery. These include avoiding strenuous activities that could impact recovery.
Light walking is often encouraged to promote blood circulation but avoid heavy lifting or vigorous exercise until cleared by your doctor.
Follow-Up Appointments
Follow-up appointments are essential for monitoring healing progress. During these visits, doctors check for signs of complications such as infection or improper healing of the wound.
These appointments also allow patients to ask questions and address concerns about their recovery process.
The full recovery timeline varies depending on the procedure’s extent and individual patient factors.
-
Minor surgeries might require only a few weeks for complete recovery.
-
More extensive procedures could necessitate several months before returning to normal activities.
The journey through understanding and addressing forehead osteoma culminates in a comprehensive exploration of its treatment options, focusing on minimally invasive and endoscopic removal techniques. These methods, including the anterior hairline incision, offer patients effective solutions with reduced recovery times and minimal scarring. The candidate evaluation process ensures that individuals receive tailored treatment plans, while post-operative care guidelines aim to facilitate a smooth recovery. This article underscores the importance of professional medical advice in choosing the most suitable approach for osteoma removal. It stresses the role of advanced surgical techniques in enhancing patient outcomes.
For those seeking further information or considering osteoma removal, consulting with a healthcare professional experienced in such procedures is crucial. They can provide detailed insights into the benefits and potential risks, helping to make informed decisions. Remember, the path to recovery starts with taking that first step towards seeking expert guidance.
Frequently Asked Questions
What is a forehead osteoma?
A forehead osteoma is a benign bone growth located on the forehead. These growths are typically slow-growing and not cancerous.
What treatment options are available for osteomas?
Treatment options include minimally-invasive surgery, endoscopic removal procedures, and traditional excision techniques. The choice depends on the size and location of the osteoma.
How does minimally-invasive surgery for osteoma work?
Minimally-invasive surgery involves smaller incisions and less tissue disruption to remove the osteoma, leading to quicker recovery times compared to traditional methods.
Can you explain the endoscopic osteoma removal procedure?
The endoscopic removal procedure utilizes a camera and specialized instruments inserted through small incisions, allowing for precise removal of the osteoma with minimal scarring.
What are some common forehead osteoma excision techniques?
Common techniques include direct excision through an anterior hairline incision or using endoscopic methods for less visible scars.
How is a candidate evaluated for osteoma removal?
Candidates undergo a comprehensive evaluation including medical history review, physical examination, and imaging studies like CT scans to determine if they’re suitable for surgery.
What does post-operative care involve after an osteoma removal?
Post-operative care includes managing pain with medications, keeping surgical sites clean, avoiding strenuous activities until cleared by your surgeon, and attending follow-up appointments for monitoring healing progress.



